Introduction
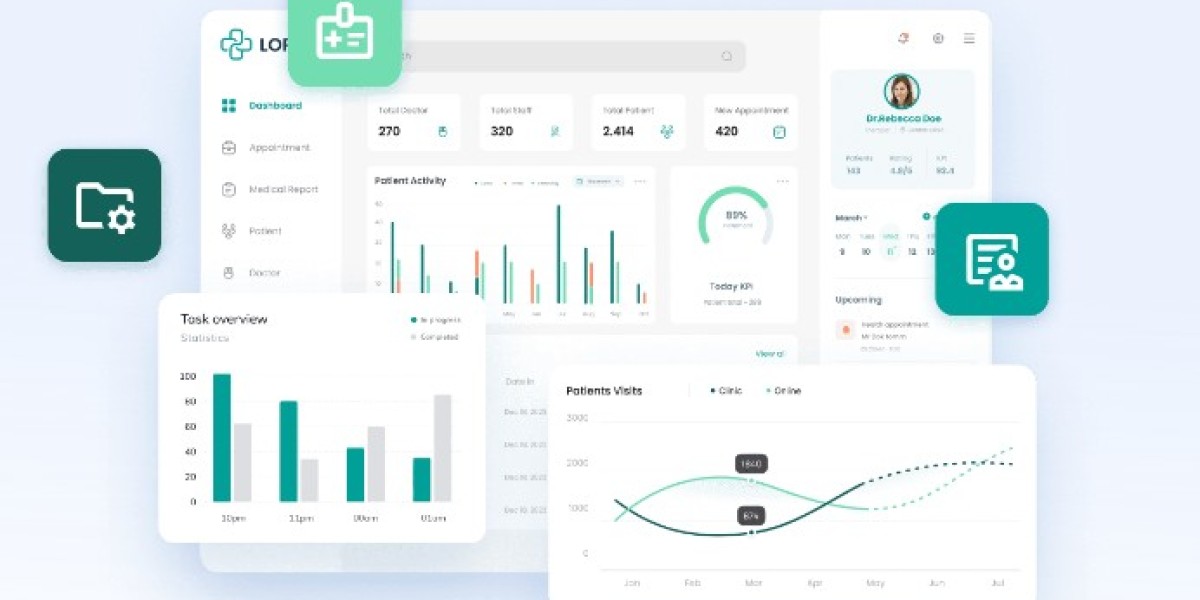
In the modern healthcare landscape, technology plays a pivotal role in enhancing patient care, streamlining operations, and improving the overall efficiency of hospitals and medical facilities. At the core of this technological evolution lies Hospital Management Software (HMS), an integrated platform that handles everything from patient records and billing to staff management and inventory control. However, with the growing reliance on software systems in healthcare, ensuring compliance with regulatory standards and safeguarding sensitive data has become paramount.
Data breaches, cyberattacks, and non-compliance with healthcare regulations can lead to dire consequences, including hefty fines, loss of reputation, and compromised patient care. As a result, developers and organizations responsible for building and maintaining hospital management software must prioritize both compliance and data security at every stage of the software development lifecycle.
This article will delve into the critical aspects of compliance and data security in hospital management software development, covering the most relevant regulatory frameworks, data protection strategies, and best practices to follow.
Understanding the Need for Compliance in Hospital Management Software
Compliance in healthcare refers to adherence to laws, regulations, and standards that govern the way healthcare providers and organizations operate. When it comes to hospital management software, ensuring compliance is crucial to:
- Protect patient privacy: Hospitals handle vast amounts of sensitive data, including personally identifiable information (PII) and protected health information (PHI). Compliance ensures that these data are handled securely.
- Mitigate legal risks: Healthcare institutions are subject to numerous legal and regulatory requirements, failure to comply with which can lead to fines, lawsuits, and penalties.
- Improve patient trust: Patients are more likely to trust healthcare providers that demonstrate a strong commitment to data security and regulatory compliance.
Key Regulatory Frameworks for Hospital Management Software
Several regulatory frameworks govern the handling of patient data and the operation of healthcare software systems. Developers and healthcare organizations must ensure that hospital management software complies with these regulations. Some of the most prominent regulatory frameworks include:
1. HIPAA (Health Insurance Portability and Accountability Act)
HIPAA, enacted in the United States, sets the standards for protecting PHI and defines the obligations of healthcare providers, insurers, and software developers who handle sensitive patient data. It has two main components:
- Privacy Rule: Establishes national standards to protect individuals' medical records and other personal health information.
- Security Rule: Sets national standards for securing electronic protected health information (ePHI).
Compliance with HIPAA requires software developers to implement measures like encryption, secure access controls, audit trails, and regular security assessments to ensure that patient data remains confidential and secure.
2. GDPR (General Data Protection Regulation)
GDPR, applicable in the European Union, governs the collection, storage, and processing of personal data, including health information. It mandates strict data protection protocols, such as:
- Data minimization: Only collect and store the data necessary for a specific purpose.
- Consent management: Ensure that patients provide explicit consent for their data to be processed.
- Data access rights: Give individuals the right to access, rectify, and erase their personal data.
Developers creating hospital management software for EU markets must ensure compliance with GDPR, especially regarding the handling of patient consent and data retention policies.
3. HITECH Act (Health Information Technology for Economic and Clinical Health Act)
The HITECH Act, closely tied to HIPAA, was enacted to promote the adoption of electronic health records (EHRs) and ensure that electronic health information is shared and used securely. The Act provides financial incentives for healthcare providers to adopt EHR systems but also increases penalties for non-compliance with HIPAA.
4. CURES Act
The 21st Century Cures Act, enacted in the U.S., aims to accelerate medical product development and facilitate faster access to new innovations in medical treatment. It includes provisions for promoting interoperability and discouraging information blocking in healthcare IT. Hospital management software must be compliant with the Cures Act to ensure interoperability between systems and avoid blocking the sharing of patient data among providers.
5. ISO 27001
ISO 27001 is an international standard for information security management. While it is not specific to healthcare, it provides a framework for ensuring data security and managing risks effectively. Developers of hospital management software can benefit from following ISO 27001 guidelines to establish a secure development process, safeguard patient data, and mitigate risks of breaches.
Data Security Challenges in Hospital Management Software
Hospital management software developers face numerous data security challenges, given the sensitive nature of healthcare information. Some of the key challenges include:
1. Cybersecurity Threats
Hospitals are prime targets for cyberattacks such as ransomware, phishing, and malware. Attackers may attempt to steal sensitive patient information or disrupt hospital operations by compromising the hospital's software systems. To counter these threats, hospital management software must incorporate robust security measures such as firewalls, intrusion detection systems, and regular security updates.
2. Data Breaches
A data breach occurs when unauthorized individuals gain access to sensitive patient data. The consequences of a breach can be devastating, both financially and in terms of patient trust. Ensuring encryption of data both at rest and in transit is crucial to prevent unauthorized access. Additionally, developers should implement role-based access controls to restrict data access to authorized personnel only.
3. Interoperability Risks
Interoperability, the ability of different healthcare systems to exchange and use data, is vital for the smooth functioning of hospital management software. However, it also introduces security risks, as data may be transmitted across multiple systems with varying security standards. Ensuring secure data exchange protocols, such as using HL7 or FHIR standards, is essential to protect patient information during transmission.
4. Human Error
Human error is one of the leading causes of data breaches in healthcare. Hospital staff may inadvertently share or expose sensitive patient information, such as by using weak passwords or falling victim to phishing scams. To mitigate this risk, developers should prioritize user-friendly security features, such as multifactor authentication, and provide training to hospital staff on cybersecurity best practices.
5. Data Storage and Retention
Hospitals generate vast amounts of data, and securely storing this data for extended periods while ensuring accessibility can be challenging. Cloud-based solutions offer scalability and flexibility, but developers must ensure that cloud storage providers comply with relevant regulations and provide secure data encryption.
Best Practices for Ensuring Compliance and Data Security in Hospital Management Software
To address the aforementioned challenges and ensure both compliance and data security in hospital management software, developers should adhere to the following best practices:
1. Conduct a Risk Assessment
Before developing or deploying hospital management software, it is essential to conduct a thorough risk assessment. This assessment should identify potential security vulnerabilities, regulatory compliance gaps, and areas where sensitive patient data could be at risk. Based on the results, developers can prioritize security measures and mitigate risks.
2. Incorporate Security by Design
Security should not be an afterthought but an integral part of the software development process. By following a "security by design" approach, developers can ensure that data protection measures are built into the software from the start. This approach includes implementing encryption, secure coding practices, and thorough testing for vulnerabilities throughout the development lifecycle.
3. Implement Encryption Protocols
Encryption is a key component of data security in healthcare software. It ensures that even if data is intercepted or accessed by unauthorized individuals, it remains unreadable. Developers should implement encryption for both data at rest (stored data) and data in transit (data being transmitted between systems).
4. Use Role-Based Access Control (RBAC)
Role-based access control (RBAC) is a security model that restricts access to sensitive information based on the user's role within the organization. For instance, administrative staff may only have access to billing information, while medical professionals can access patient medical records. Implementing RBAC ensures that only authorized personnel can view or modify sensitive data.
5. Regular Security Audits and Updates
Hospital management software should undergo regular security audits to identify and address vulnerabilities. Cyber threats evolve constantly, so it's essential to keep software systems updated with the latest security patches. Automated vulnerability scanning tools can be used to detect and mitigate potential security risks.
6. Ensure Compliance with Interoperability Standards
To promote data exchange between different healthcare systems securely, developers should adhere to established interoperability standards, such as HL7 (Health Level 7) and FHIR (Fast Healthcare Interoperability Resources). These standards ensure that data can be shared between systems without compromising security.
7. Provide User Training on Data Security
Even the most secure hospital management software can be compromised by human error. Developers should collaborate with healthcare institutions to provide user training on cybersecurity best practices. Training should cover topics such as identifying phishing attempts, using strong passwords, and the importance of secure data sharing.
8. Implement Multi-Factor Authentication (MFA)
Multi-factor authentication (MFA) adds an extra layer of security by requiring users to verify their identity through multiple factors (e.g., a password and a one-time code sent to their phone). This significantly reduces the risk of unauthorized access to hospital management systems, even if a user's password is compromised.
9. Ensure Data Backup and Recovery Systems
Data loss, whether due to a cyberattack, system failure, or natural disaster, can have severe consequences in a hospital setting. Developers should implement robust data backup and recovery systems to ensure that patient data can be restored in case of an emergency. Backups should be encrypted and stored securely to prevent unauthorized access.
Conclusion
Ensuring compliance and data security in hospital management software development is essential for protecting patient privacy, safeguarding sensitive health information, and adhering to regulatory requirements. By following best practices, such as conducting risk assessments, incorporating security by design, and implementing encryption and access controls, developers can create robust and secure systems that enable hospitals to