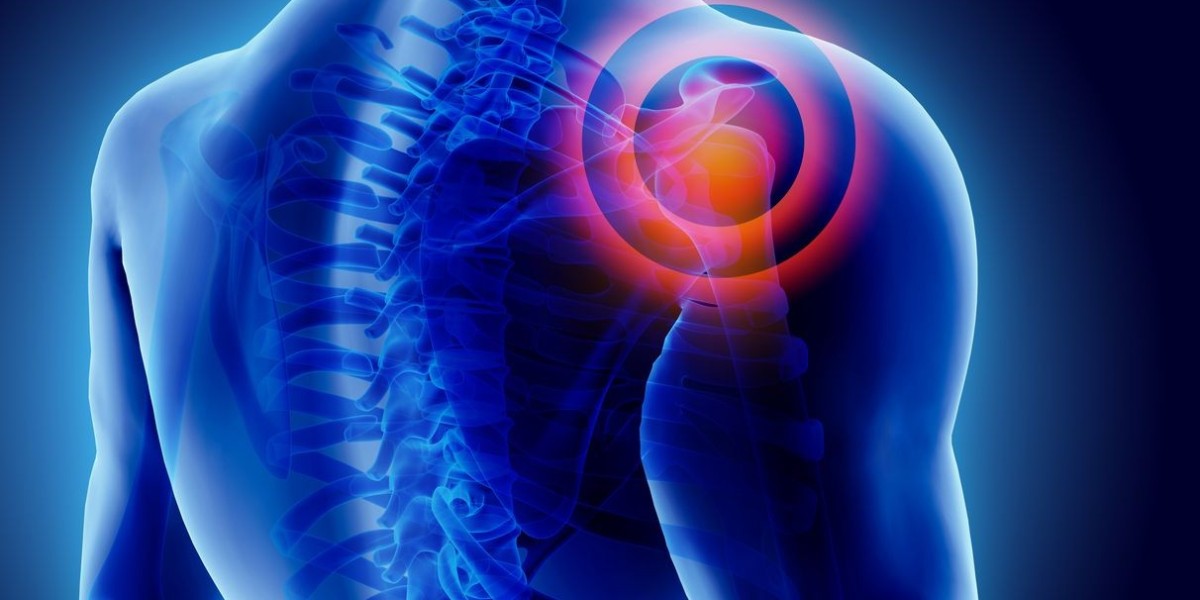
Pain is a universal experience, but its nature and management can vary widely. Understanding the difference between acute and chronic pain is crucial for effective treatment and improving quality of life. This article explores the types of pain, their underlying causes, and various treatment options available.
Understanding Pain: Acute vs. Chronic
Acute Pain: The Immediate Response
Acute pain treatments is a direct response to injury, illness, or other types of trauma. It is typically sharp and sudden, and it serves as a warning signal to the body that something is wrong. This type of pain usually lasts for a short duration, ranging from a few moments to a few weeks, depending on the severity of the underlying cause. Common examples include:
Sprains, fractures, and cuts.
Post-operative pain.
Earaches or dental pain.
Chronic Pain: The Persistent Challenge
Chronic pain is defined as pain that persists beyond the usual course of acute illness or injury, often lasting for months or even years. Unlike acute pain, which diminishes as the body heals, chronic pain can continue even after the initial cause has resolved. It can be continuous or intermittent and varies in intensity. Chronic pain often impacts daily life, emotional well-being, and overall quality of life. Examples include:
Joint pain and stiffness.
Persistent pain in the lower or upper back.
Widespread muscle pain and tenderness.
Diagnosing Pain: Tools and Techniques
Accurate diagnosis is essential for effective treatment. Physicians use a variety of tools and techniques to determine the type and source of pain:
Detailed patient history helps identify the onset, duration, and nature of the pain.
Assessing physical symptoms and functionality.
X-rays, MRI, and CT scans to visualize internal structures.
Blood tests to check for underlying conditions or infections.
Tools like the Visual Analog Scale (VAS) or McGill Pain Questionnaire to quantify pain levels and characteristics.
Treatment Strategies for Acute Pain
Pharmacological Interventions
Medications like ibuprofen or aspirin reduce inflammation and pain.
Effective for reducing pain and fever, though it doesn’t address inflammation.
For severe pain, although they are used with caution due to the risk of addiction and side effects.
Non-Pharmacological Interventions
Applying ice and resting the affected area to reduce swelling and pain.
For muscle pain and stiffness, applying heat can improve blood flow and alleviate discomfort.
Tailored exercises and treatments to improve mobility and strength.
Treatment Strategies for Chronic Pain
Pharmacological Interventions
Certain antidepressants can help manage chronic pain by altering pain perception and improving mood.
Medications originally designed for epilepsy, such as gabapentin, can also help with nerve pain.
Creams and patches applied to the skin can provide localized pain relief.
Non-Pharmacological Interventions
A psychological approach to help patients manage pain by changing their thought patterns and behaviors.
Focuses on exercises and techniques to improve function and reduce pain.
An alternative therapy involving the insertion of thin needles into specific points on the body to alleviate pain.
Practices such as meditation and deep breathing can help manage the emotional and physical aspects of chronic pain.
Integrative Approaches and Lifestyle Adjustments
Diet and Nutrition
A balanced diet can play a significant role in managing pain. Anti-inflammatory foods, such as those rich in omega-3 fatty acids (e.g., fish, flaxseeds), antioxidants (e.g., fruits and vegetables), and whole grains can help reduce pain and inflammation. On the other hand, excessive intake of processed foods and sugars may exacerbate pain symptoms.
Exercise and Physical Activity
Regular exercise can improve physical function and reduce pain levels in both acute and chronic conditions. Low-impact activities like swimming, walking, or yoga can help maintain joint flexibility and muscle strength without putting undue stress on the body.
Sleep and Rest
Quality sleep is essential for pain management. Poor sleep can exacerbate pain and interfere with the body’s healing processes. Establishing a regular sleep routine and creating a comfortable sleep environment can significantly impact pain levels and overall health.
When to Seek Professional Help
While many instances of acute pain resolve with home treatment, persistent or severe pain should be evaluated by a healthcare professional. Similarly, chronic pain that significantly impacts daily life warrants a comprehensive approach involving specialists such as pain management doctors, physical therapists, or psychologists. Early intervention and a multidisciplinary approach can improve outcomes and enhance quality of life.
Conclusion
Navigating pain, whether acute or chronic, requires a nuanced understanding of its nature and effective treatment strategies. Acute pain often resolves with time and appropriate treatment, while chronic pain necessitates a more complex and sustained approach. By leveraging a combination of pharmacological, non-pharmacological, and integrative methods, individuals can manage pain more effectively and improve their overall well-being. Seeking professional guidance when needed ensures that pain is addressed comprehensively, paving the way for a better quality of life.