A fracture, commonly known as a broken bone, occurs when the continuity of the bone is disrupted due to trauma, stress, or disease. Fractures vary widely in severity and type, ranging from minor cracks to complete breaks, and can affect any bone in the body. While fractures are often caused by accidents, they can also occur from repetitive stress or underlying medical conditions such as osteoporosis. The ability of bones to heal depends largely on the nature of the fracture, the treatment received, and the patient's overall health. Diagnosing a fracture correctly is critical to ensure the proper treatment and recovery process.
Types of Fractures and Their Causes
Fractures can be classified into several types depending on the way the bone breaks and the underlying cause. Simple or closed fractures occur when the bone breaks but does not penetrate the skin, while compound or open fractures involve a break that protrudes through the skin, increasing the risk of infection. Stress fractures are small cracks in the bone that develop over time due to repetitive activity or overuse, common among athletes. Pathological fractures occur in bones weakened by diseases such as cancer or osteoporosis, making them more prone to breaking under minor stresses. Understanding the type of fracture is vital as it informs the treatment plan and potential recovery timeline.

Symptoms of Fractures and How They Present
The most common symptoms of fractures include severe pain at the site of injury, swelling, bruising, and an inability to move the affected area. In some cases, visible deformity may occur, especially in compound fractures where bone protrudes through the skin. The severity of the symptoms often correlates with the severity of the fracture, although in some cases, such as with hairline fractures, the pain may be mild initially but worsen over time. It is also possible for fractures to cause additional complications such as nerve or blood vessel damage, which may present as numbness, tingling, or loss of circulation in the affected limb.
How Fractures Are Diagnosed Initial Assessment
The initial assessment of a suspected fracture begins with a physical examination by a healthcare provider. The doctor will examine the affected area for signs of swelling, deformity, or abnormal movement and will ask the patient about the circumstances surrounding the injury. The patient's medical history is also crucial, as preexisting conditions such as osteoporosis or previous fractures can influence the diagnosis. In some cases, physical manipulation may be used to assess the stability of the bone, but this is done cautiously to avoid causing further damage.
Diagnostic Imaging Techniques X-rays and Beyond
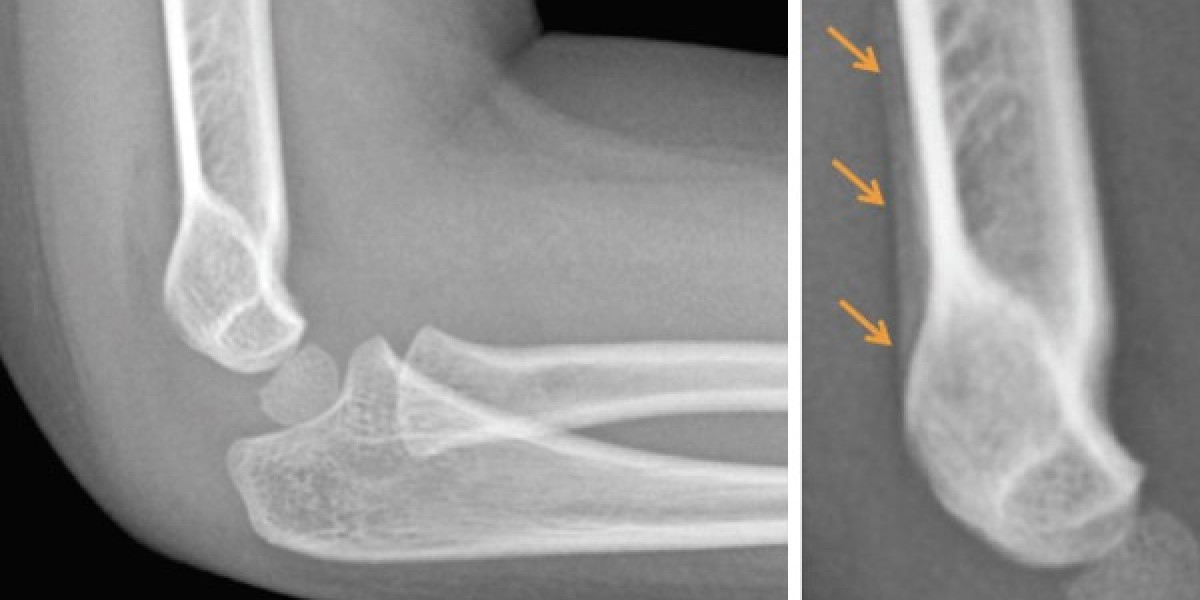
Imaging techniques play a pivotal role in diagnosing fractures, as they allow the doctor to see inside the body without surgery. The most common and widely available imaging tool is the X-ray, which can clearly show most types of fractures. X-rays are quick, inexpensive, and provide detailed images of bone structure. However, in cases where more detail is needed, such as with stress fractures or complex injuries involving multiple bones, advanced imaging techniques may be used. A CT (computed tomography) scan provides cross-sectional images that offer more detail about the extent of the fracture and any associated soft tissue damage. MRI (magnetic resonance imaging) is often employed to detect stress fractures or fractures not visible on X-rays, as it provides detailed images of both bones and soft tissues.
Bone Scans Detecting Hidden Fractures
In some cases, fractures may not be immediately visible on X-rays or other imaging tests. This is especially true for stress fractures or those occurring in bones that are difficult to image, such as the spine. A bone scan may be recommended in these situations. During a bone scan, a small amount of radioactive material is injected into the bloodstream, which accumulates in areas of high bone activity, such as healing fractures. This technique is highly sensitive and can detect fractures that might otherwise be missed, making it a valuable tool for diagnosing stress injuries or fractures in complex areas like the pelvis.
Other Diagnostic Tools Ultrasound and Physical Testing
In certain cases, additional diagnostic tools such as ultrasound may be used to assist in identifying fractures. While ultrasound is not typically used for diagnosing fractures in the bone itself, it can be helpful in assessing surrounding tissues like muscles, tendons, and ligaments. Additionally, physical tests like the "tuning fork test," in which a vibrating fork is placed on the bone, can sometimes help identify fractures, particularly stress fractures. The vibration causes increased pain if a fracture is present due to the sensitivity of the broken bone.
Treatment of Fractures Based on Diagnosis
Once a fracture is diagnosed, the treatment approach will depend on the type, severity, and location of the fracture. Most fractures are treated with immobilization using a cast or splint, allowing the bone to heal in the correct position over time. In more severe cases, surgical intervention may be necessary to realign the bones or insert pins, plates, or rods to stabilize the fracture. Physical therapy is often required during the recovery process to restore strength and mobility in the affected area. Early and accurate diagnosis of fractures is crucial to ensure appropriate treatment and prevent long-term complications such as chronic pain or improper healing.
Conclusion
Fractures are a common but serious injury that requires proper diagnosis and treatment for effective recovery. Understanding the different types of fractures, their causes, and symptoms is essential for recognizing when medical attention is needed. Diagnostic tools such as X-rays, CT scans, MRI, and bone scans play a vital role in determining the extent of the injury, allowing healthcare providers to create a tailored treatment plan. Timely diagnosis and appropriate care can significantly improve outcomes, reducing the risk of complications and ensuring a quicker return to normal activities.
FAQs
What are the most common causes of fractures?
Fractures are most commonly caused by trauma such as falls, car accidents, or sports injuries. They can also result from repetitive stress or conditions like osteoporosis that weaken the bones.
How long does it take for a fracture to heal?
The healing time for fractures varies depending on the type and severity of the break, but most fractures take six to eight weeks to heal, with more complex fractures requiring longer recovery times.
Can fractures heal without treatment?
While some minor fractures may heal without medical intervention, most fractures require treatment to ensure the bones heal correctly. Without proper treatment, fractures can lead to complications like improper healing or chronic pain.
What is the difference between a fracture and a break?
A fracture and a break are the same thing. Both terms refer to a disruption in the continuity of the bone, although "break" is often used colloquially, while "fracture" is the medical term.
Can you still walk on a fractured bone?
Walking on a fractured bone depends on the location and severity of the fracture. In some cases, a person may be able to walk with a minor fracture, but this can worsen the injury. It is best to avoid putting weight on the affected limb until diagnosed by a healthcare professional.